Part One: Sensory Engagement
The Namaste Care Programme is a strengths-based and person-centred model of palliative and end-of-life care. It was originally developed by Joyce Simard for people with advanced dementia but is now increasingly recognised as being valuable for people with a range of life-limiting conditions.
Take some time to watch and consider the following videos. Each has a slightly different perspective on Namaste Care. As you watch you might hold the following questions in your mind.
What do you notice?
What questions do you have… what do you wonder?
What insights and realisations do you notice bubbling up?
1) It’s about the food not the fork – sensory engagement and creating beautiful (5 mins)
2) Understanding Sensory Changes in Dementia
Ian James takes about the importance of recognising sensory changes that come with dementia
Watch here
3) Sharing Sensory Stories and Conversations with People with Dementia
A fascinating book (Lorna loves it) and an inspiring, thought-provoking chat with the author.
Watch here
5) Creating a Sense and Sensory Environment Profile
The Sense and Sensory Environment Profile helps identify what residents enjoy and value across the five senses: touch, taste, smell, sight, and sound.
Read here
6) Universal Human Needs
What needs have been met by browsing through resource on sensory engagement? Your own needs – the needs of others?
Read here
Part Two: How might we watch for cues that sensory engagement practices are welcome and wanted – or not?
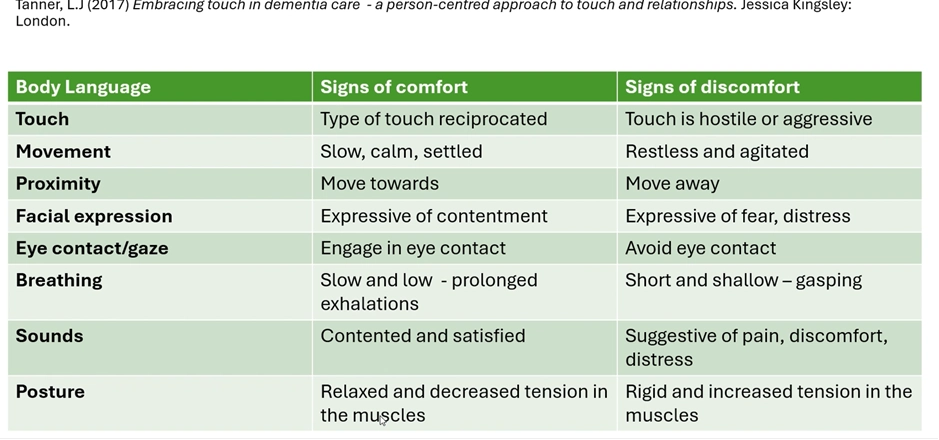
It is vital to be aware that people with dementia can still express preferences and choices. We should be alert to verbal, behavioural or emotional signals that express preferences and choices. This will help ensure we are offering sensory engagement practices that are wanted and welcome. It will also ensure we notice the verbal, behavioural and/or emotional signals that they are not wanted or welcome at that time – and we immediately stop.
1) Core principles to consider when offering sensory engagement practices to people with cognitive impairment (including comforting touch)
Comforting Touch Principles
Watch here
2) What did you do, what was the impact?
From pages 55 & 56 Namaste Care Guidance for Care Homes
Read here
Noticing and Amplifying ‘Glimmers ’
- How might you consider the important topics of respecting preferences and choices your care setting?
- Would the principles discussed in the video help?
- Could the questionnaire developed by the University of Worcester help?
Part Three: How can I purposefully use my voice to soothe and comfort in Namaste Care?
Some hints and tips from Lorna
In my experience, growing your voice takes time. It requires patience, a lot of self-kindness, and a willingness to experiment—one thing at a time.
From many years of reading to my children and guiding mindfulness meditations, here are a few of my own hints and tips.
First of all, find some voices you enjoy. I’m drawn to voices with a soothing, warm quality. Here are some voices I enjoy -
Consider – what do I like about these voices.
At the same time start practicing reading aloud.
Start small – children’s pictures books are great for this. I love Frog and Toad.
Take your time.
Relax a little. Smile a little.
Leave space and pause.
Part Four: What is your soundscape like?
Carry out a soundscape evaluation here
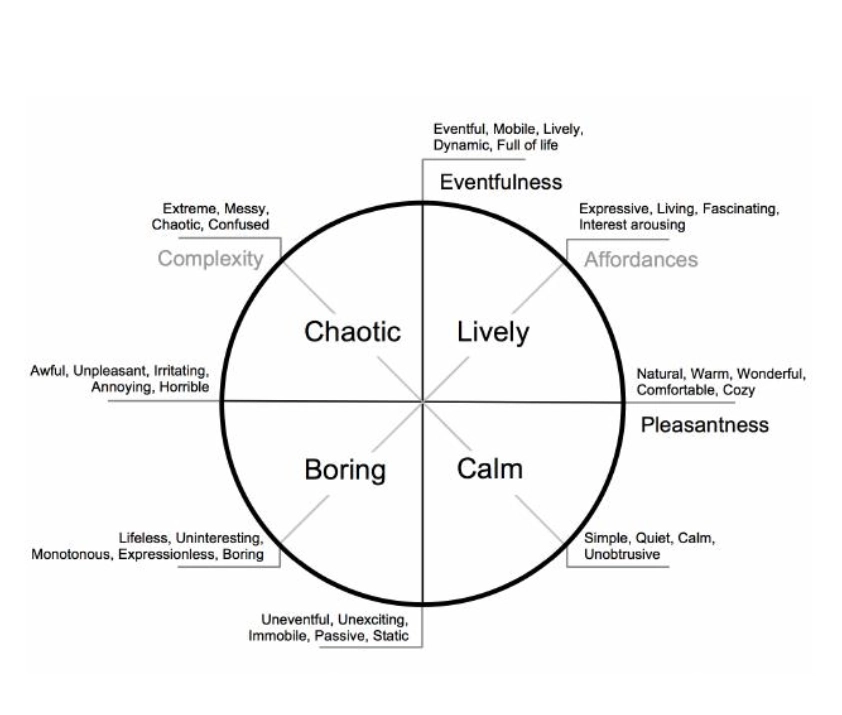
Care homes are places filled with the buzz of everyday life. They can be places of peace and quiet, as well as busyness and bustle.
The purpose of this Care Home Sound Scape resource is to help us to tune into the sounds in care homes, particularly sounds that we have become so used to, that we may no longer hear. For example, the sound of friendly banter in the distance, or a dishwasher being emptied, or outside noises such as birds or traffic.
By becoming more familiar with all the everyday sounds of the care home, it may help us to become more aware of what the experience might be like for residents of being in the lounge, or their bedroom, or other areas in the home.
Becoming more familiar with the care home soundscape may offer clues as to sounds and noises that residents find enjoyable, soothing, confusing or uncomfortable.
The Sound Scape Activity could be carried out by staff, a visitor or a resident.
1) How would you describe the soundscape in your care setting at the moment?
2) What could you do to change it for the better?
3) What do you know now that you did not know before watching, reading and listening to the items in this section?
4) What difference will knowing that make to you, to your practice of Namaste Care?
Part Five: The M-Technique – and other ways to offer positive comforting touch
1) Reflect on the last time you were with a person with dementia. Recall when you touched that person. Would you describe your motivation as being mainly function based (to carry out personal care, to accompany someone to the toilet or the dining room etc) or mainly comfort based (to reassure, to accompany, to communicate empathy, to lend comfort)?
2) How often to employ stillness in your touch – e.g. holding a hand?
3) How often to you offer choreographed touched which aims to comfort and soothe?
Teepa Snow: touch permission, touch tolerance and the need for touch
Watch here
Demonstration of the M-Technique
Watch here
Article: The Power of Touch
Read here
E-book – Touch in the Helping Professions
Read here
Part Six: Music and Silence
Fiona offers some thoughts around music and dementia
Watch here
Dementia UK: Music and dementia blog
Read here
Teepa Snow on Connecting Through Music in Dementia Care
Watch here
Former Ballerina With Alzheimer's Performs Swans Lake
Watch here
How the Magic of Music Can be Therapeutic for People with Dementia
Watch here
Alive Inside: Full film
Watch here
Playlist for Life website
Read here
Part Seven: Pain and Dementia
Information from Dementia UK
Read here
Information from Alzheimer Scotland
Read here
Video: the OUCH campaign
Watch here
Pain assessment PAIN AD tool
Read here
Pain and dementia
Watch here
Delirium and depression in dementia
Watch here
Managing distressed behaviours
Watch here
Some possible causes of distress in the hospital setting
Watch here
What is your experience of supporting someone with pain and dementia?
What has helped?
What do the resources in this section add to your knowledge?
How will you use this knowledge – what difference will it make?
Part Eight: Anticipatory Grief – Understanding Grief and Helping and Supporting People Experiencing Anticipatory Grief
Anticipatory Grief Animation
Watch here
Julia Samuel Anticipatory Grief
Watch here
How to cope with Anticipatory Grief
Watch here
Loss Grief and bereavement in dementia factsheet
Read here
Ambiguous loss, Dr. Pauline Boss
Watch here
Tips for Dementia Caregiving
Watch here
What stands out from the videos in this section?
What will you do more of after watching any video in this section?
What will you do less of?