Part One: The Development of Lorna and Fiona’s Namaste Care Work — and Thinking — Over the Years
Looking Closer
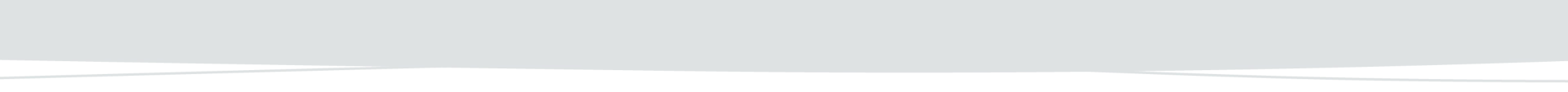
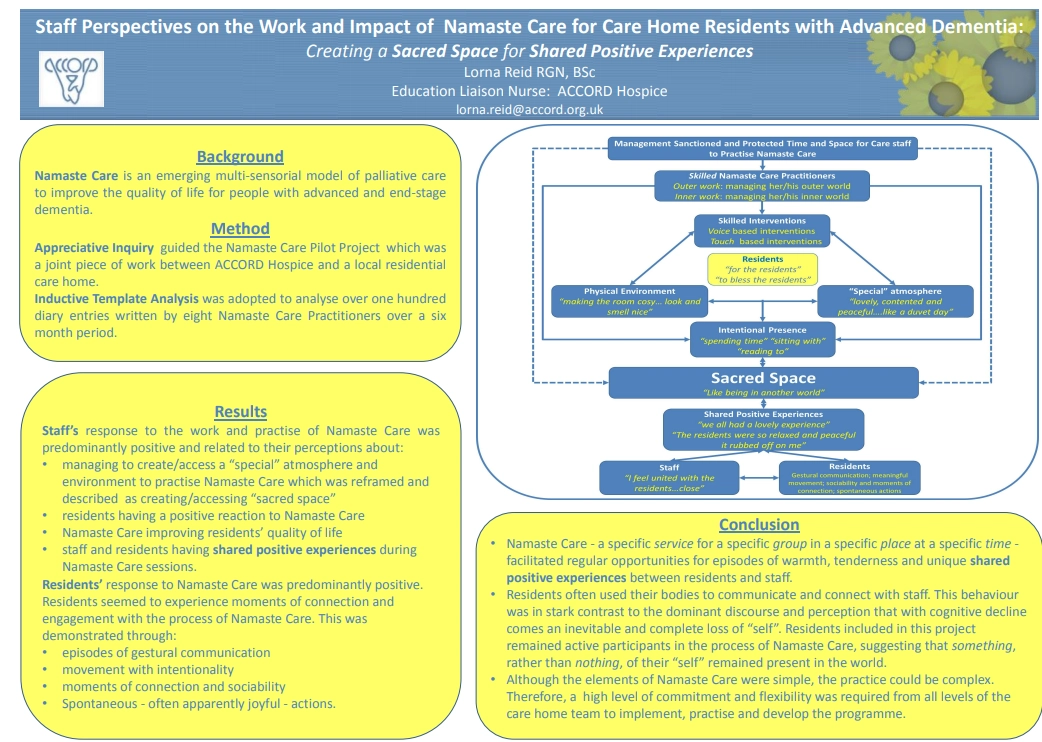
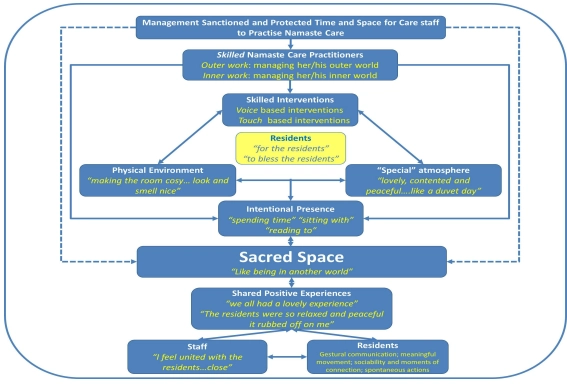
During the first Namaste Care project in Scotland, Lorna identified four essential layers of ‘holding’ that contributed to its success:
Firstly: The sanctioning of protected time and space for Namaste Care to take place — this is the holding provided by management.
Secondly: The skill of Namaste Care practitioners — managing both the outer world (room setup, atmosphere, sensory practices) and the inner world (presence, emotions, thoughts). This is the holding offered by the practitioner.
Thirdly: The sensitive and appropriate delivery of the sensory engagement practices — this is the holding within the practices themselves.
And finally: The holding of a warm, compassionate intention — to ‘bless’ and benefit the residents through a positive mindset.
When holding was present across all these layers, staff were able to create and inhabit a special, even sacred, space with residents — a space where everyone could benefit.
Reflection
Take a moment to assess your readiness to offer Namaste Care effectively. These questions can help guide your thinking and next steps:
- Do you have the support of management? If not, what small steps can you take to begin changing that?
- Do you feel able to manage your outer environment well enough for Namaste Care to take place? If not, what small steps can you take to begin making that possible?
- Do you feel able to manage your inner environment well enough for Namaste Care to take place? If not, what small steps can you take to make improvements?
(Consider using glimmers, STOP, 5-4-3-2-1, or talking to someone about your concerns.) - Do you feel confident in the sensory engagement practices you learned during the workshop series? If not, can you start small to build your confidence?
Can you revisit the resources from Day Two and choose one area to focus on and practice more? - Do you remind yourself daily of your intention for practicing Namaste Care? If not, would it help to write it down somewhere visible as a regular reminder?
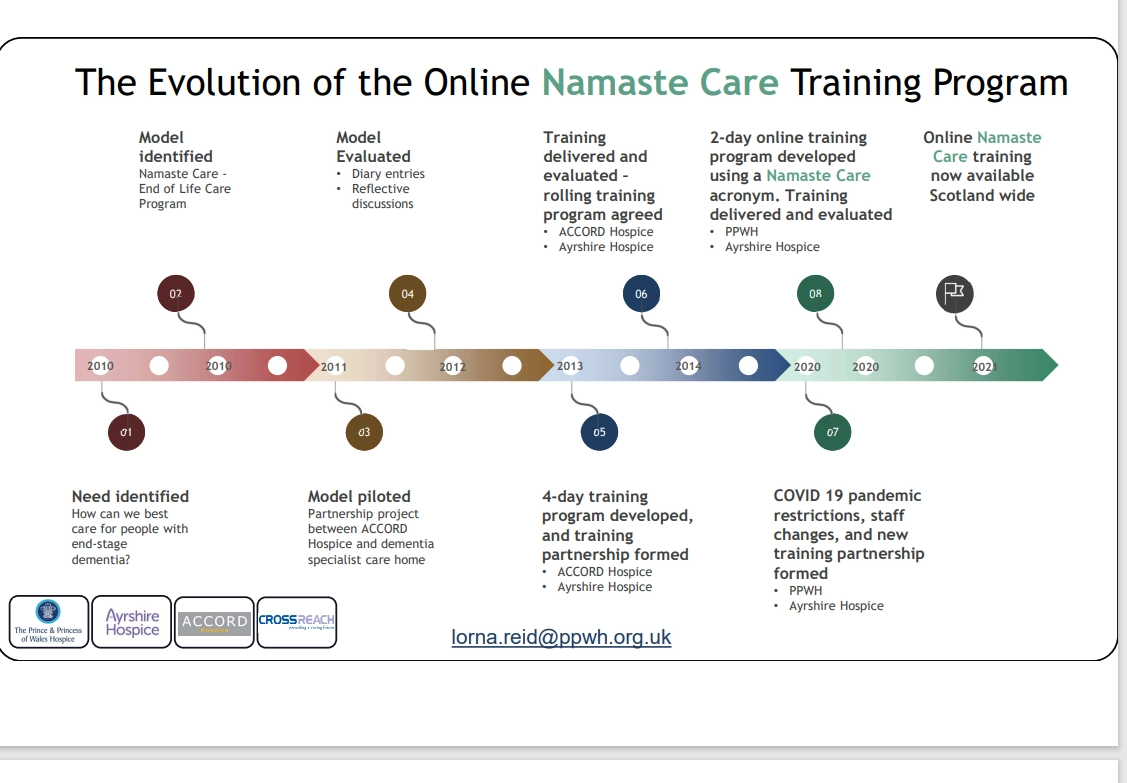
The work continued…

The pandemic came, and the work developed and went online…
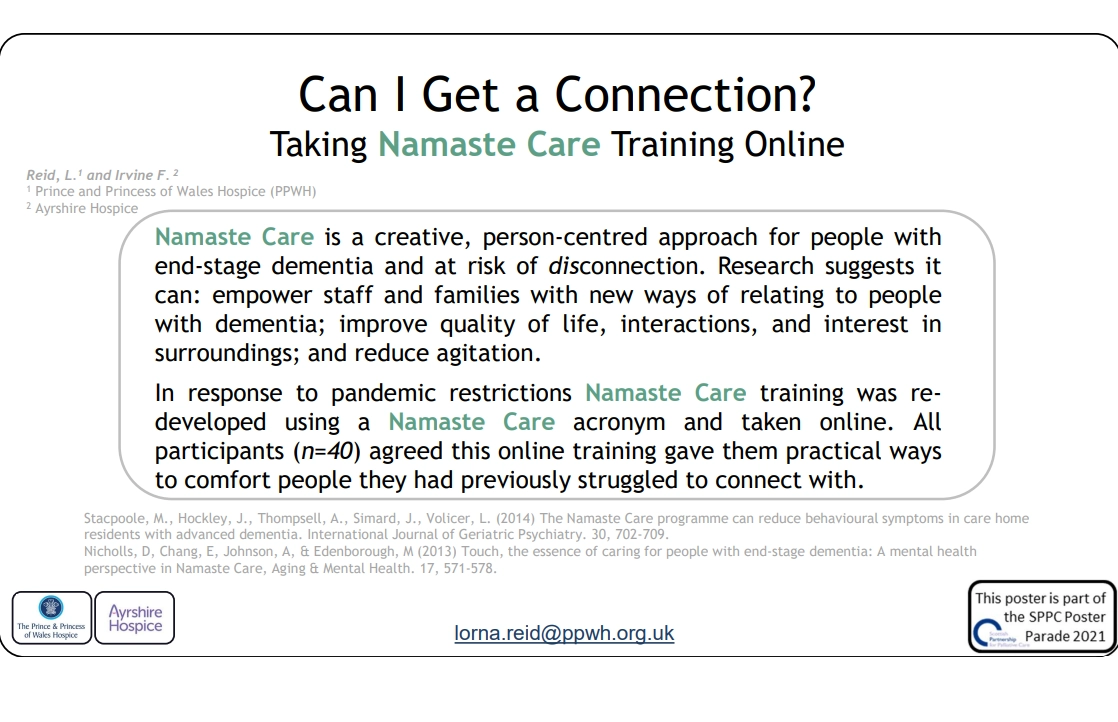
NAMASTE CARE – Hospice UK Conference
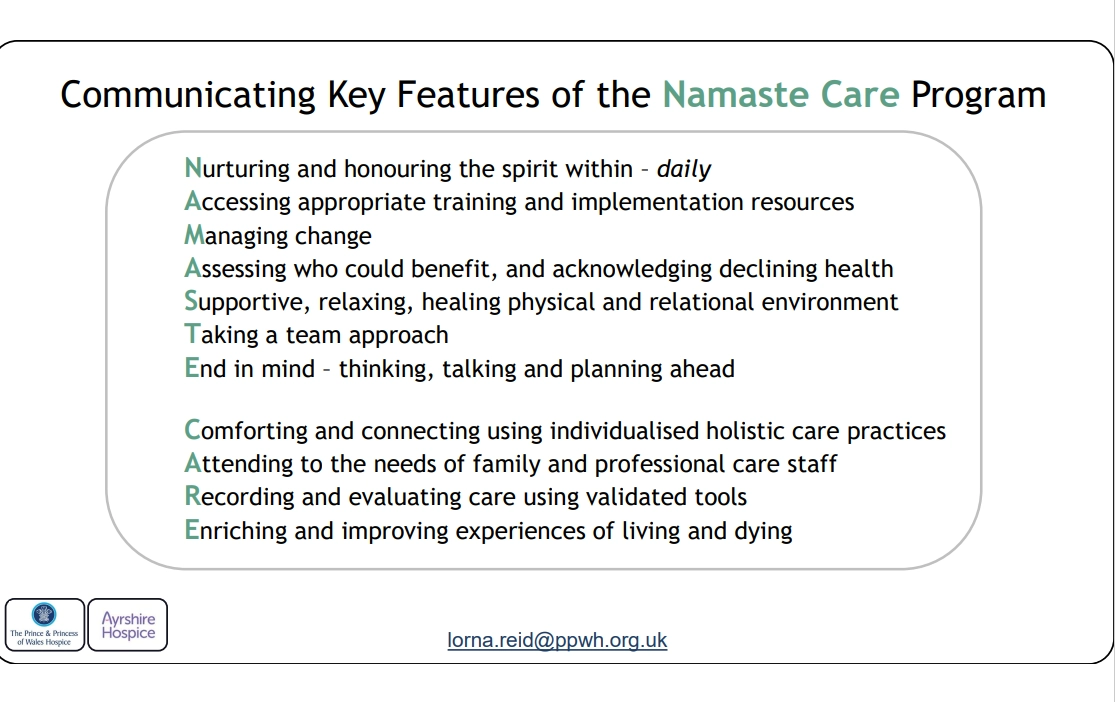
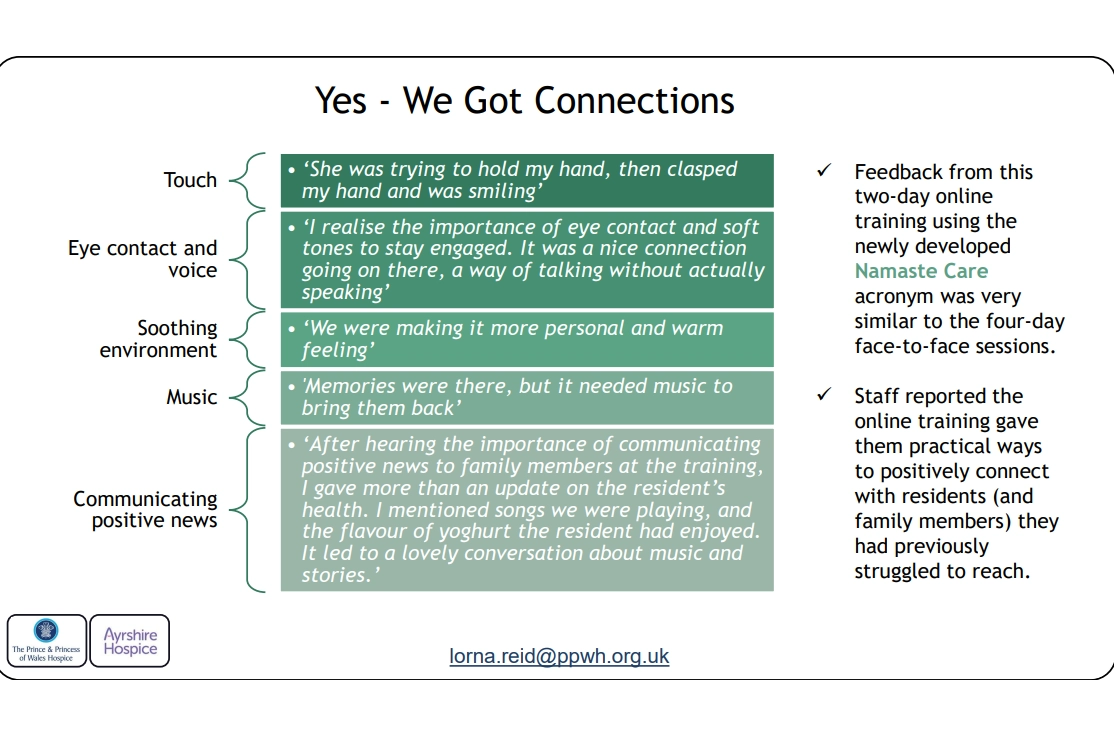
Most recently, we created a descriptive participant feedback story structured around the letters of NAMASTE CARE. This was presented at the Hospice UK conference, highlighting the importance of connecting Namaste Care with conversations about future care planning.
Reflection
- What catches your eye as you read the stories shared in the poster?
- What resonates with your own experience of Namaste Care so far?
- What additional hints or tips can you take from the poster and stories?
Part Two: How Namaste Care Has Been Adopted, Adapted, and Researched in the UK
The first UK research was conducted by the care home team from St. Christophers Hospice, in London.
You can hear Min Stackpoole talk about that work.
Watch here
Read about the research here:
Read here
During the workshops, we heard about the work of Kimberly St. John. You can find out more about her research on implementing Namaste Care in a hospital setting.
Read here
We heard about “Namaste Care on the Go” from Emma Biglands, an occupational therapist from Tees, Esk and Wear Valleys. Emma generously shared her case study with us.
Read here
We heard about the work of Emily Brown, the first Namaste Care Practitioner within an NHS hospital setting. The hospital has recently announced the opening of a dedicated Namaste Care Room.
View here
New room created to deliver UK’s first Namaste care service in a hospital setting
Read more
Here is a short video of Emily speaking about her work
Watch here
We heard about Nicola Kendall's amazing work with volunteers. You can read more about that work in her books.
View here
You can hear her speak about Namaste Care and what she is doing now.
Watch here
We heard from Lesley Wylie — you can read more about her and her QNIS project.
Read here
You can read about the research conducted by the University of Worcester.
Read here
Read about the research from the University of Lancaster
Read here
Part Three: Resources to Help You Implement Namaste Care
Part Four: With the End in Mind
Here is a link that explains why noticing changes in health matters, and how SPICT can help us review a person’s care and make realistic plans for the future.
View here
Here is a link to SPICT4ALL, a simplified version of the tool that uses clear, non-clinical language.
View here
Here is a link to SPICT, designed for use by healthcare staff.
View here
Here is a link to a video about future care planning that could be helpful for family members and friends when introducing the topic.
Watch here
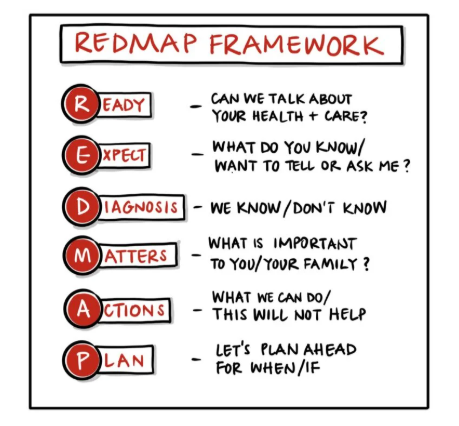
The REDMAP framework is a six-step guide for future care planning conversations with or about people living with long-term conditions and disabilities, or older adults who are becoming more frail. It was developed by Dr. Kirsty Boyd, Reader in Palliative Care at the University of Edinburgh. This framework can help you think about how to approach conversations regarding the future care of individuals whose condition is deteriorating.
View here
Preparing for Meaningful Conversations
Before beginning a conversation, it can be helpful to reflect and make a list to keep your goals in mind. This list might include:
- Building rapport with the person.
- Exploring their understanding of the current situation — their health and any health issues.
- Gathering the following:
- Their ideas about the situation
- Their concerns and worries
- Their hopes and expectations for what might happen next
- Sensitively sharing information about the person’s condition, including:
- The fact of declining health
- The reality of deterioration
- The likelihood that recovery is unlikely
- The uncertainty around how quickly things may change
- Finding out what matters most to the person — "If time were short, what would matter most to [name], and what would matter most to you?"
- Offering empathy, kindness, and support.
- Discussing comfort-focused care and what can continue to be done well.
- Exploring future scenarios and discussing realistic options together.
- Creating a future care plan that centres the person, their wishes, comfort, and realistic choices.
Here is a link to help you guide conversations with families and friends.
View here
Achieving dignity at the end of life in dementia.
Watch here
How Does a Person Die from Dementia.
Watch here
5 Signs of Approaching Death (Dr. Paulien Moyaert)
Watch here
Namaste Care for a person who is dying.
View here
Reflection
Before using tools like SPICT or RED-MAP, it can be valuable to reflect on your personal experiences and current practices. Consider the following questions:
- What is your experience of caring for someone at the end of their life?
- What would your own wishes be — for yourself, or for someone you care about?
- Have you known someone whose wishes were quite different from your own?
(e.g. not wanting anyone with them when they die; wanting all their family around, which might feel a bit chaotic to you; not wanting a funeral; wishing to donate their body for research) - How do those experiences leave you feeling?
- What tools do you currently use to help you notice changes in a person’s condition within your care setting?
- Could SPICT help?
- What framework do you currently use to help you talk to people about changes in their condition, find out what matters most to them, and discuss what will or will not help?
- Do you consider your goals before you have such a conversation? Do you think writing some goals down could help?
- Could RED-MAP help?
Part Five: Noticing How We Feel, Completing the Stress Cycle, and Caring for Each Other
Your Wellbeing Matters
Each one of us is important and valuable.
We all deserve to feel well — not just so we can care for others, but because we are important in our own right. It’s essential to include ourselves in our own circle of care.
Sometimes, we might feel a bit like this:

Or like this:
Reflection
How are you feeling right now?

Do you notice any signs or symptoms of excessive stress?

Who is aware of how you're feeling right now?
Could you speak with someone about it?
Can you recognise what you're already doing to care for yourself — and take a moment to acknowledge and celebrate that?
Could you enhance each of the five pillars of wellbeing by just 1% today?

Are you experiencing any of the following signs of burnout?
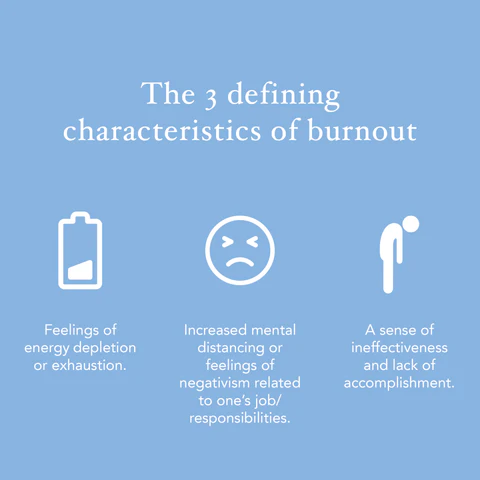
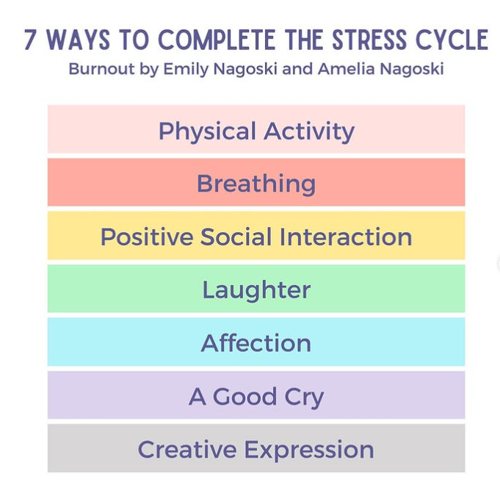
If so, consider watching this talk on stress and burnout. It explains how completing the stress cycle can be more effective than simply practising 'self-care'.
Emily Nagoski and Amelia Nagoski: The Cure for Burnout (Hint: It Isn't Self-Care) | TED
7 Ways to Complete the Stress Cycle
Final Thoughts